A Case of Status Epilepticus on CEEG
- Callie Klotka
- Nov 15, 2023
- 4 min read
This is the case of a 69 year old male who presented via ambulance after having an unwitnessed cardiac arrest and being down for an unknown period of time. The patient arrives at the ER via ambulance using life saving measures such as CPR, medications, and AED. Upon arrival at the ER it was discovered that the patient had suffered from a catastrophic cardiac arrest. The patient is unresponsive and admitted to the ICU. Once stabilized, it is noted that the patient has some mild jerking. A continuous EEG is ordered to identify if this patient has an ongoing neurological issue due to lack of oxygen to the brain, or a hypoxic anoxic event.
The CEEG has begun and the background shows suppression with low amplitude bursts of theta every 15-20 seconds.

After about 3 minutes of monitoring the patient shows signs of seizure activity with associated jerking. The onset of these seizures is fast activity followed by increased EMG.

This activity quickly evolved into 10-12 hz spike and wave activity that continued for 25 seconds before beginning to slow to 3 hz spike and polyspike wave activity

This activity slows to 2 hz before abrupt abatement of activity. Following this event is a suppressed background.

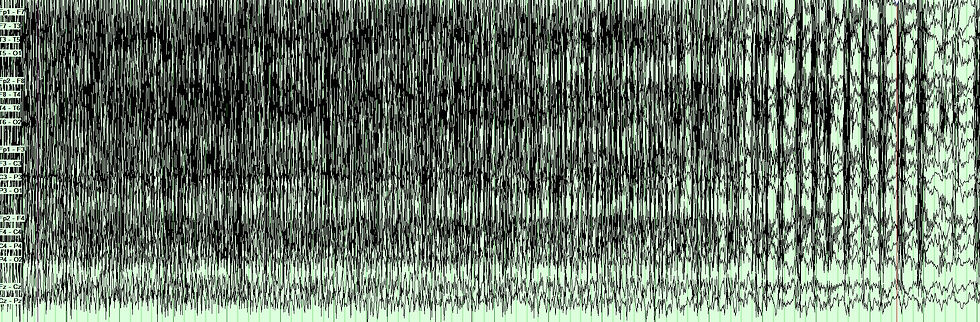
The event lasts for 2 minutes and 15 seconds in duration. Within 2 minutes time the EEG shows another event with an identical beginning, middle, end, and duration. This pattern continues for the next couple of hours as they work to treat the patient. The patient is suffering from a seizure burden of 12-15 seizures per hour lasting 2-3 minutes in duration or As the staff enters the room and begins facilitating treatment for the patient; the increased patient stimulus only increases the activity on EEG. The EEG changes again to show continuous 3-4 hz spike and polyspike wave activity for over 10 minutes before slowing to continuous, but variable frequency of 1-4 hz, spike wave for another 45 minutes indicating status epilepticus.

The patient is loaded with Ativan, Depakote, Keppra, and finally Propofol to induce burst suppression. Burst suppression was achieved after 78 minutes of status epilepticus. The background continues as low amplitude bursts every 4-6 seconds with low amplitude bursts of delta/theta for the next several hours.

During noxious stimuli by staff there is an increase in background activity and bursts of generalized spikes originating from the central region.

The EEG remains connected through the following day as sedation was lifted. The background continues to show burst suppression with increased duration, amplitude, and frequency of the bursts.

During stimulation the EEG continues to show stimulus induced generalized spike and polyspike and wave discharges with an increased background frequency. After several hours off of sedation and with stimulus to the patient the EEG shows an increase in spikes and ultimately results in a generalized tonic clonic ictal activity lasting 3 minutes in duration followed by low amplitude diffuse slowing.
This is the end of the tonic clonic activity seen above.

The EEG was disconnected shortly after this clip and after the MD spoke to the family about comfort care. As remote EEG technologists we don’t always have a chance to hear the outcome however, we do see a lot of interesting and thought provoking cases.
What do we know about status epilepticus and how do we readily identify it?
Status epilepticus is a medical emergency. The Neurocritical Care Society guidelines from 2012 revised the definition to a seizure with 5 minutes or more of continuous clinical and/or electrographic seizure activity or recurrent seizure activity without recovery between seizures.[1][2][3][4] This needs to be identified and treated as soon as possible to prevent significant morbidity or mortality.
Status epilepticus can be caused by CNS infections, metabolic issues, stroke, head trauma, hypoxia, autoimmune disease, drug or alcohol withdrawal, and drug toxicity both prescription and illicit. Inside the brain there is an excessive amount of excitatory neurotransmitters and/or inadequate inhibitory neurotransmitters leading to uncontrolled electrical discharges of the neurons.
The first line medications for rapid treatment of status epilepticus are benzodiazepines which increase GABA’s ability to bind to the receptor and open the chloride channels to inhibit the excited neurons. Second line treatment includes an AED like phenytoin, valproate, or levetiracetam to keep the seizures at bay. Third line treatment generally is reserved for refractory status epilepticus. These include sedatives like Propofol, Ketamine, Midazolam, or Pentobarbital.
Status epilepticus should be treated rapidly; it only takes 30 minutes before there could be permanent neurologic damage from this event. The treatment team for status epilepticus should include nursing, neurology, and a quick pharmacy turnaround for best patient outcomes.
In the case I have shared today we know that this patient was in the ICU with a hypoxic or anoxic brain injury causing over excitement of the neurons, in combination with the catastrophic cardiac arrest and unknown down time; the prognosis for the patient was poor and was only more evident with the development of status epilepticus.
As EEG technologists we hold the power to quick effective treatment for our patients, we have the power to save a life and help improve patient outcomes and safety especially in the ICU! I hope that this helps current and future techs in recognizing and understanding status epilepticus and the importance of rapid communication with our neurologists.
1. Xu MY. Poststroke seizure: optimising its management. Stroke Vasc Neurol. 2019 Mar;4(1):48-56. [PMC free article] [PubMed]
2.Horváth L, Fekete I, Molnár M, Válóczy R, Márton S, Fekete K. The Outcome of Status Epilepticus and Long-Term Follow-Up. Front Neurol. 2019;10:427. [PMC free article] [PubMed]
3. Peng P, Peng J, Yin F, Deng X, Chen C, He F, Wang X, Guang S, Mao L. Ketogenic Diet as a Treatment for Super-Refractory Status Epilepticus in Febrile Infection-Related Epilepsy Syndrome. Front Neurol. 2019;10:423. [PMC free article] [PubMed]
4. Ramos AB, Cruz RA, Villemarette-Pittman NR, Olejniczak PW, Mader EC. Dexamethasone as Abortive Treatment for Refractory Seizures or Status Epilepticus in the Inpatient Setting. J Investig Med High Impact Case Rep. 2019 Jan-Dec;7:2324709619848816. [PMC free article] [PubMed]




Comentarios